Dt. Kanika Khanna is a professional Kidney Disease Management Dietitian in Lawrence Road having 14+ years of experience. We are known as Best Kidney Disease Management Diet Consultant in Lawrence Road. So, You can visit Top Most Verified Kidney Disease Management Diet Clinic in Lawrence Road. Book Appointment Online for Kidney Disease Management Diet in Lawrence Road.

Kidney Disease Management Diet Consultant in Lawrence Road, Dietitian for Kidney Disease in Lawrence Road, Nutritionist for Kidney Disease in Lawrence Road, Dietician for Kidney Disease in Lawrence Road. Many people with mild or chronic kidney disease are not even aware of their disorder.
Kidney disease is a 'silent killer' as it generally evolves over time, and in many cases, patients cannot notice the early signs and symptoms of the Kidney Disorder.
Dietitian Kanika Khanna in Lawrence Road will help you Whether you are in the earlier stages of kidney disease, on dialysis or living with a kidney transplant, or have diabetes or high blood pressure with kidney disorders, you need a healthy lifestyle and therapeutic renal diet to manage the symptoms and to help live a longer and healthier life. We are experts in diet and nutrition specifically for people with kidney disease like acute and chronic kidney disease, kidney stones, dialysis, kidney transplant or polycystic kidneys. We closely monitor your kidney blood parameters and plan diet accordingly. Since there are lots of restriction in renal diet we get to know your food habits and preferences, and can work with you to create a meal plan that you will want to follow when at home or out.
Dietofy team emphasizes fishing the cause of illness rather than just reducing the symptoms. We recommend how to eat healthy for your stage of kidney disease, so you may be able to slow down or stop the progression to kidney failure.
Patient education
If you are on dialysis, your dietitian will likely recommend how much fluid you should consume each day to control fluid buildup in your blood between treatments. If you also have diabetes or high blood pressure, your dietitian should help you tailor your diet, so you are eating the right way for all of your conditions.
If you are post-transplant, it is still important to follow your dietitian's guidelines because they will help you keep your new kidney healthy. You may have a different eating plan that is high in protein directly after surgery to help you recover. You may also need to adjust the nutrients you consume based on how your body tolerates anti-rejection medicines. Your dietitian can help you adjust to any changes you need to make for the life of your transplant.
If you are unsure if something is healthy for you, it is a good idea to check with your dietitian at your next appointment before consuming it.
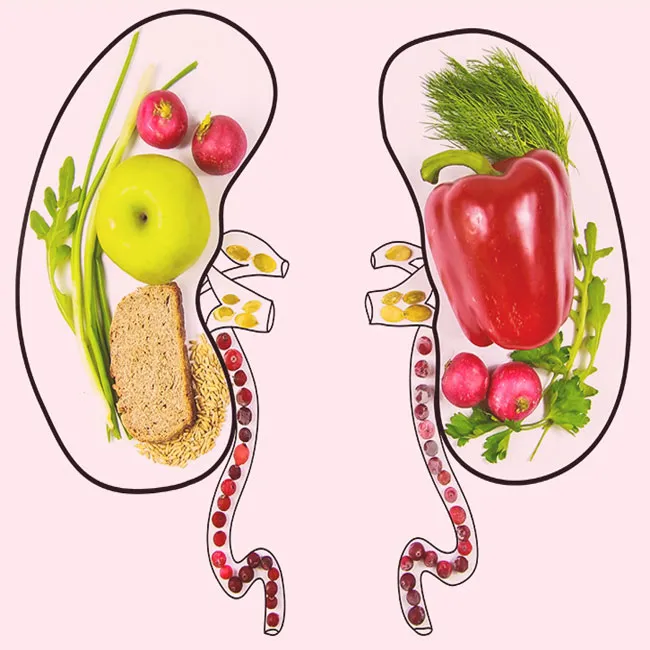
People with compromised kidney function must adhere to a renal or kidney diet to cut down on the amount of waste in their blood. Wastes in the blood come from food and liquids that are consumed. When kidney function is compromised, the kidneys not filter or remove waste properly. If waste is left in the blood, it can negatively affect a patient's electrolyte levels. Following a kidney diet in Lawrence Road may also help promote kidney function and slow the progression of complete kidney failure.
A renal diet in Lawrence Road is one that is low in sodium, phosphorous, and protein. A renal diet in Lawrence Road also emphasizes the importance of consuming high-quality protein and usually limiting fluids. Some patients may also need to limit potassium and calcium. Every person's body is different, and therefore, it is crucial that each patient works with a renal dietitian work to come up with a diet that is tailored to the patient's needs.
Below are some substances that are crucial to monitor to promote a renal diet:
Sodium
 What is Sodium and its role in the body?
What is Sodium and its role in the body?
Sodium is a mineral found in most natural foods. Most people think of salt and sodium as interchangeable. Salt, however, is actually a compound of sodium and chloride. Foods we eat may contain salt or they may contain sodium in other forms. Processed foods often contain higher levels of sodium due to added salt.
Sodium is one of the body's three major electrolytes (potassium and chloride are the other two). Electrolytes control the fluids going in and out of the body's tissues and cells. Sodium contributes to:
• Regulating blood pressure and blood volume
• Regulating nerve function and muscle contraction
• Regulating the acid-base balance of blood
• Balancing how much fluid the body keeps or eliminates
Why should kidney patients monitor sodium intake?
Too much sodium can be harmful for people with kidney disease because their kidneys cannot adequately eliminate excess sodium and fluid from the body. As sodium and fluid build up in the tissues and bloodstream, they may cause:
• Increased thirst
• Edema: swelling in the legs, hands, and face
• High blood pressure
• Heart failure: excess fluid in the bloodstream can overwork your heart, making it enlarged and weak
• Shortness of breath: fluid can build up in the lungs, making it difficult to breathe
How can patients monitor their sodium intake?
• Always read food labels. Sodium content is always listed.
• Pay close attention to serving sizes.
• Use fresh, rather than packaged meats.
• Choose fresh fruits and vegetables or no-salt-added canned and frozen produce.
• Avoid processed foods.
• Compare brands and use items that are lowest in sodium.
• Use spices that do not list "salt" in their title (choose garlic powder instead of garlic salt.)
• Cook at home and do NOT add salt.
• Limit total sodium content to 400 mg per meal and 150 mg per snack.
Printable Low Sodium Diet Guidelines (PDF)
Potassium
What is Potassium and its role in the body?
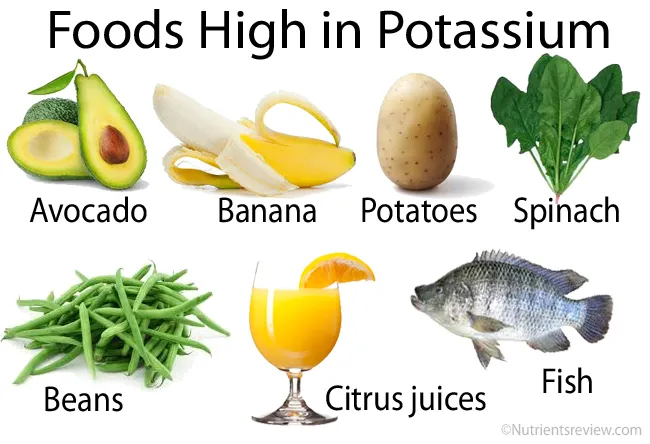
Potassium is a mineral found in many of the foods we eat and is also found naturally in the body. Potassium plays a role in keeping the heartbeat regular and the muscles working correctly. Potassium is also necessary for maintaining fluid and electrolyte balance in the bloodstream. The kidneys help to keep the right amount of potassium in your body and they expel excess amounts into the urine.
Why should kidney patients monitor their potassium intake?
When the kidneys fail, they can no longer remove excess potassium, so potassium levels build up in the body. High potassium in the blood is called hyperkalemia which can cause:
• Muscle weakness
• An irregular heart beat
• Slow pulse
• Heart attacks
• Death
How can patients monitor their potassium intake?
When the kidneys no longer regulate potassium, a patient must monitor the amount of potassium that enters the body.
 Tips to help keep the levels of potassium in your blood safe, make sure to:
Tips to help keep the levels of potassium in your blood safe, make sure to:
• Talk with a renal dietitian about creating an eating plan.
• Limit foods that are high in potassium.
• Limit milk and dairy products to 8 oz per day.
• Choose fresh fruits and vegetables.
• Avoid salt substitutes & seasonings with potassium.
• Read labels on packaged foods & avoid potassium chloride.
• Pay close attention to serving size.
• Keep a food journal.
Printable Low Potassium Diet Guidelines (PDF)
Phosphorus
What is Phosphorus and its role in the body?
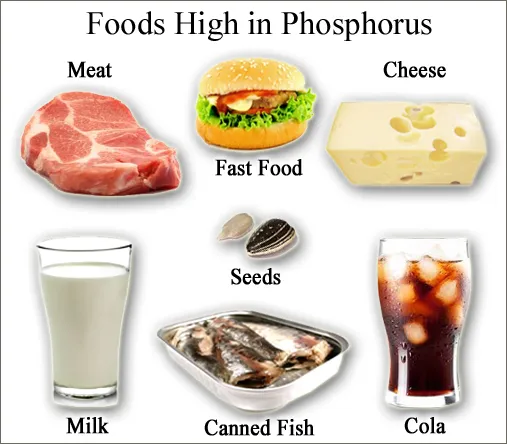
Phosphorus is a mineral that is critical in bone maintenance and development. Phosphorus also assists in the development of connective tissue and organs and aids in muscle movement. When food containing phosphorus is consumed and digested, the small intestines absorb the phosphorus so that it can be stored in the bones.
Why should kidney patients monitor Phosphorus intake?
Normal working kidneys can remove extra phosphorus in your blood. When kidney function is compromised, the kidneys no longer remove excess phosphorus. High phosphorus levels can pull calcium out of your bones, making them weak. This also leads to dangerous calcium deposits in the blood vessels, lungs, eyes, and heart.
How can patients monitor their Phosphorus intake?
Phosphorus can be found in many foods. Therefore, patients with compromised kidney function should work with a renal dietitian to help manage phosphorus levels.
 Tips to help keep phosphorus at safe levels:
Tips to help keep phosphorus at safe levels:
• Know what foods are lower in phosphorus.
• Pay close attention to serving size
• Eat smaller portions of foods that are high in protein at meals and for snacks.
• Eat fresh fruits and vegetables.
• Ask your physician about using phosphate binders at meal time.
• Avoid packaged foods that contain added phosphorus. Look for phosphorus, or for words with "PHOS" on ingredient labels.
• Keep a food journal
Printable Low Phosphorus Diet Guidelines (PDF)
Protein
 Protein is not a problem for healthy kidneys. Normally, protein is ingested and waste products are created, which in turn are filtered by the nephrons of the kidney. Then, with the help of additional renal proteins, the waste turns into urine. In contrast, damaged kidneys fail to remove protein waste and it accumulates in the blood.
Protein is not a problem for healthy kidneys. Normally, protein is ingested and waste products are created, which in turn are filtered by the nephrons of the kidney. Then, with the help of additional renal proteins, the waste turns into urine. In contrast, damaged kidneys fail to remove protein waste and it accumulates in the blood.
The proper consumption of protein is tricky for Chronic Kidney Disease patients as the amount differs with each stage of disease. Protein is essential for tissue maintenance and other bodily roles, so it is important to eat the recommended amount for the specific stage of disease according to your nephrologist or renal dietician.
Fluids
Fluid control is important for patients in the later stages of Chronic Kidney Disease because normal fluid consumption may cause fluid build up in the body which could become dangerous. People on dialysis often have decreased urine output, so increased fluid in the body can put unnecessary pressure on the person's heart and lungs.
 A patient's fluid allowance is calculated on an individual basis, depending on urine output and dialysis settings. It is vital to follow your nephrologist's/nutritionist's fluid intake guidelines.
A patient's fluid allowance is calculated on an individual basis, depending on urine output and dialysis settings. It is vital to follow your nephrologist's/nutritionist's fluid intake guidelines.
To control fluid intake, patients should:
• Not drink more than what your doctor orders
• Count all foods that will melt at room temperature (Jell-O®, popsicles, etc.)
• Be cognizant of the amount of fluids used in cooking
Monitoring your health
Your renal dietitian conducts a regular nutrition assessment for you and monitors your lab work, medicines and weight, so they can make recommendations for you during each visit. They also monitor your blood pressure and adjust your eating plans as needed to control it. They know that what you consume not only affects your kidneys, but your overall health.
If you are on dialysis, your dietitian likely monitors your dry weight and weight between appointments to determine how well the treatments are working for you. If you need to lose weight before transplant surgery, your dietitian can also help you with that.
If you are post-transplant, your dietitian likely recommends that you to stick to a low-sodium meal plan to help control your blood pressure. They should make sure you are consuming well-balanced foods and drinks that help you keep a healthy weight, are good for your overall health and work well with your immunosuppressive medicines. They can also teach you and your and caregiver about food safety to help avoid infections and minimize any bacteria that can get into your body from food.
Following your renal dietitian's recommendations is one of the best things you can do for your overall health. For more information on kidney-friendly eating, kidney-friendly recipes, sample grocery shopping lists, nutrient trackers and more, visit Kidney Kitchen®.
FILED UNDER
• Healthy living
• Living with kidney disease
• Nutrition
• Diet
Kidney disease, also known as renal disease is much more widespread that people realize. It often goes undetected and undiagnosed until it is well advanced. People usually realize that they have kidney diseases when it is down 25% of the normal. As kidney disease advances, the organ's function is severely impaired and dangerous level of fluid and waste can build up in body in no time. It is important that people who suffer from or are at high risk of developing kidney disease, get their kidney functions regularly checked. Early detection may help prevent serious kidney damage.
Common symptoms include high blood pressure, blood in urine, and fatigue
People with compromised kidney function must adhere to a renal or kidney diet to cut down on the amount of waste in their blood. Wastes in the blood come from food and liquids that are consumed. When kidney function is compromised, the kidneys not filter or remove waste properly. If waste is left in the blood, it can negatively affect a patient's electrolyte levels. Following a kidney diet may also help promote kidney function and slow the progression of complete kidney failure.
A renal diet is one that is low in sodium, phosphorous, and protein. A renal diet also emphasizes the importance of consuming high-quality protein and usually limiting fluids. Some patients may also need to limit potassium and calcium. Every person's body is different, and therefore, it is crucial that each patient works with a renal dietitian as per patient's needs.
Protein:
Protein is not a problem for healthy kidneys. Normally, protein is ingested and waste products are created, which in turn are filtered by the nephrons of the kidney. Then, with the help of additional renal proteins, the waste turns into urine. In contrast, damaged kidneys fail to remove protein waste and it accumulates in the blood.
The proper consumption of protein is tricky for Chronic Kidney Disease patients as the amount differs with each stage of disease. Protein is essential for tissue maintenance and other bodily roles, so it is important to eat the recommended amount for the specific stage of disease according to your nephrologist or renal dietician.